Medicine is advancing rapidly, with new technologies and treatment modalities being developed to meet the unique needs of patients. These modalities range from personalized medicines like specific compounding to cell and gene therapies, based on the patients individual genome, that promise to target hereditary diseases.
New combination products, new delivery systems, and novel excipients that play an essential role in how well a drug works in the body are also being developed at speeds never seen before.
In addition, digital therapeutics – medical treatments delivered via software on a phone or tablet – have the potential to help patients prevent, manage, or treat a wide range of physical, mental and behavioral conditions.
Precision medicine, which considers genetic, environmental and lifestyle factors, could mean quality standards need to evolve to account for variables that are not considered in a “fit-for-all” model of medicine. Below are some examples of the work USP is engaged in with stakeholders to explore pathways different from USP’s traditional standard-setting processes.
Oligonucleotides:
Genomics:
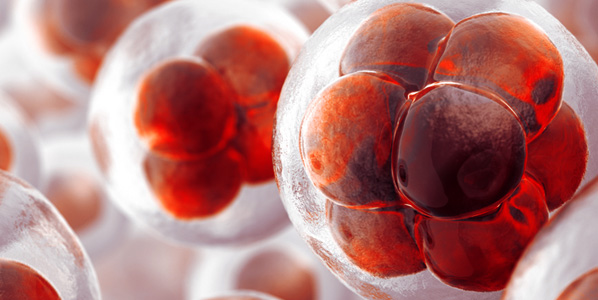
Cell and gene therapies and gene editing:
Compounding preparations:
Novel vaccine platforms and adjuvants that may increase trust in the development of new vaccines:
- The Role of Standards in Supporting Quality Vaccines Manufacturing and Distribution
- Accelerating Development and Building Trust in COVID-19 Vaccines With Public Quality Standards
Digital therapeutics that may decrease the use of drugs or completely eliminate them for certain health conditions:
- Quality Concerns and Future Steps into the Era of “Digital Medicines”
- The role of public standards in assuring quality of digital therapeutics
Nanomedicines that may better target disease sites, sparing healthy cells and tissues:
Microbiome therapeutics (live bio-therapeutics) like strain-specific probiotics that could be used to aid in a variety of health conditions: